Version of Record (VoR)
Osuagwu, U. L., Chikasirimobi, T. G., Langsi, R., Abu, E. K., Goson, P. C., Mashige, K. P., … Agho, K. E. (2021). Differences in perceived risk of contracting SARS-CoV-2 during and after the lockdown in Sub-Saharan African countries. International Journal Of Environmental Research And Public Health, 18(21). https://doi.org/10.3390/ijerph182111091
Differences in Perceived Risk of Contracting SARS-CoV-2 during and after the Lockdown in Sub-Saharan African Countries
Citation: Osuagwu, U.L.; Timothy C.G.;. Langsi, R.; Abu, E.K.; Mashige, K.P.; Ekpenyong, B.; Miner, C.A.; Oloruntoba, R.; Ishaya, T.; Envuladu, E.A.; et al. Differences in Perceived Risk of Contracting SARS-CoV-2 during and after the Lockdown in Sub-Saharan African Countries. Int. J. Environ. Res. Public Health 2021, 18, x. https://doi.org/10.3390/xxxxx
Academic Editor(s): Jimmy T. Efird
Received: 7 October 2021
Accepted: 18 October 2021
Published: date
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Copyright: © 2021 by the authors. Submitted for possible open access publication under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
1 Translational Health Research Unit (THRI), School of Medicine, Western Sydney University, Campbelltown, NSW 2560, Australia
Abstract:
This study investigated risk perception in sub-Sahara Africa during and after the lockdown of contracting and dying of SARS-CoV-2. Two online surveys were conducted one year apart, with participants 18 years and above living in sub-Sahara Africa or the diaspora. Each survey took four weeks. The first survey was taken from 18 April to 16 May 2020, i.e., during the lockdown. The second survey was taken from 14 April to 14 May 2021, i.e., after the lockdown. A cross-sectional study using adopted and modified questionnaires for both surveys were distributed through online platforms. Question about risks perception of contracting and dying of SARS-CoV-2 were asked. The Helsinki declaration was applied, and ethical approvals were obtained. Total responses for both surveys, i.e., both during and after the lockdown, was 4605. The mean age was similar in both surveys (18–28 years). The mean risk perception scores were higher after lockdown by 3.59%. Factors associated with risk perception of COVID-19 were survey period, age group, region of residence, and occupation. Non-health care workers had a lower risk perception of COVID-19. This first comparative study on the level of risk perception of Africans during and after the lockdown shows that one in every three and every four persons in sub-Sahara Africa felt at high risk of contracting COVID-19 and thought they could die from contracting the same, respectively.
Keywords: SARS-CoV-2; sub-Sahara Africa; risks perception
1. Introduction
Since SARS-CoV-2, a beta coronavirus genre more closely linked to the SARS-CoV-1 (79% sequence identity) than to the MERS-CoV (52% identity) [1], was declared a pandemic by WHO in 2020 [2], the virus has infected over 237 million people, with the death of no less than 4,839,000 people, with US being the worst-affected country recording 727,273 deaths, followed by Brazil—599,414 deaths, India—449,883 deaths, Mexico—279,894 deaths, and Russia—212,625 deaths, as of 7 October 2021. In Africa, South Africa—87,981, Tunisia—24,971, Egypt—17,531, and Morocco—14,390 account for the highest number of deaths from COVID-19 in the region [3]. The SARS-CoV-2 infection presents with dry cough, fever, dyspnea, and lung trouble, among other signs [4]. With no effective cure or current drug for the treatment of the infection insight, SARS-CoV-2 continues to be a source of concern across the globe and more so in sub-Saharan Africa considering the poor health care system [5]. The rollout of the vaccines has been anything but smooth due to the mixed messages from the various governments and the difficulty in accessibility for developing countries [6,7]. This increases the mistrust displayed by citizens across the globe and increases the perception of risk in the community [7]
In sub-Saharan Africa (SSA), the impact of SARS-CoV-2 has remained minimal compared to the Americas, Europe, and Asia; however, there has been an increase in COVID-19 deaths across Africa since mid-July 2021.§ Although the reasons for this are not well understood, researchers have suggested that the demographic age structure of sub-Saharan Africa is the leading factor of the low morbidity and mortality of COVID-19 compared to other regions of the world [8]. Other factors, such as the lack of long-term care facilities, potential cross-protection from previous exposure to circulating coronaviruses, and low testing of SARS-CoV-2, have resulted in an undercounting of deaths and effective government public health responses have contributed to the lower burden of the disease [8]. According to data from the US Centers for Disease Control and Prevention (CDC), 80% of COVID-19-related deaths occur in individuals aged 65 years and older [9], with UK data demonstrating that advanced age is the strongest risk for death and dramatically outweighs the risks associated with any other demographic factor or medical condition [10]. The median age of the SSA population is considerably lower than other regions, with a median age of 18 and only 3.0% of the African population older than 65 years [11,12]
South Africa has one of the highest infection and deaths rates due to COVID-19 in Africa. In addition, countries have already implemented the recommended public health regulations, such as strict, partial, or full lockdown procedures [4]; social distancing; mask-wearing in public places; and vaccination rolled out in the majority of the SSA countries. Countries that embarked on total lockdown were avoiding any national resurgence. Wide-scale domestic, foreign, and religious events have been cancelled for fear of SARS-Cov-2 outbreak as they were considered super-spreaders of the virus [13,14]. Such actions have an enormous socio-economic impact on the country [15], and the shutdown has upstretched fears of economic repercussions [16]. Due to this pandemic, everything about human life, including exports and imports of goods, business, infrastructural development, agriculture, and education, seem to have stopped, and these have a direct and indirect negative effect on the economy [17] given the already weak economy of some SSA countries and the resultant drawback risks.
In South Africa, a study showed that a higher perceived risk of COVID-19 infection was associated with greater depressive symptoms and, with such high rates of severe mental illness coupled with the low availability of mental healthcare amidst COVID-19 in the region, there is a need for studies to understand if the change in time has any effect on the level of risk perception for targeted intervention, including the need for immediate and accessible psychological resources [18]. In our recent study conducted during the early lockdown, SSA displayed high individual risk perception scores, which was greater in older participants and those working in health care sectors after adjusting for covariates [19]. It is unclear whether similar risk perceptions and associated factors remain after participants have grown in their knowledge of the disease spread and the commencement of the vaccine rollout in most SSA countries. The current study aims to investigate the individual perception of risk for contracting SARS-Cov-2 and the associated factors by comparing the data obtained during lockdown with those obtained in the post-lockdown period in SSA. The findings of this study will provide an understanding of the population at higher risk for which can be used to implement emergency policies to counter the spread of SARS-Cov-2.
2. Materials and methods
2.1. Data collection
An e-link to the survey was disseminated via emails and posted on social media platforms (Facebook and WhatsApp) and was available for four weeks at each period (during the lockdown and after lockdown). Of the 4605 participants for both the first and second survey, 4572 provided responses on their place of origin and out of these numbers, and 4551 mentioned their countries in SSA and were included in the analysis. Internal procedures during the data collection explained the small difference in the number of participants between the two surveys (n = 2,001, vs. n = 2,550). Table 1 provides details about the sociodemographic characteristics of the participants and health status.# The questionnaire included a brief overview of the context, purpose, procedures, nature of participation, privacy and confidentiality statements, and notes to be filled out [20].
Table 1. Sociodemographic characteristics of respondents in both surveys.
| Demographics | Total (N = 4551) |
During Lockdown (n = 2001) |
Post-Lockdown (n = 2550) |
|---|---|---|---|
| Age category in years | |||
| 18–28 years | 1697 (38.0) | 774(39.1) | 923 (37.2) |
| 29–38 | 1242 (27.8) | 526 (26.5) | 716 (28.9) |
| 39–48 | 939 (21.1) | 439 (22.2) | 500 (20.2) |
| 49+ years | 584 (13.1) | 242 (12.2) | 342 (13.8) |
| Sex | |||
| Males | 2467 (54.5) | 1095 (55.2) | 1372 (53.8) |
| Females | 2057 (45.5) | 889 (44.8) | 1168 (45.8) |
| SA Region of Origin | |||
| West Africa | 2572(56.5) | 1122 (56.1) | 1450 (56.9) |
| East Africa | 347(7.6) | 212 (10.6) | 135 (5.3) |
| Central Africa | 570 (12.5) | 253 (12.6) | 317 (12.4) |
| Southern Africa | 1062 (23.3) | 414 (20.7) | 648 (25.4) |
| Country of residence | |||
| Africa | 4250 (93.6) | 1852 (92.6) | 2398 (94.4) |
| Diaspora | 291 (6.4) | 149 (7.4) | 142 (5.6) |
| Marital Status | |||
| Married/de facto | 2003 (44.3) | 876 (44.1) | 1127 (44.4) |
| Not married † | 2522 (55.7) | 1112 (55.9) | 1410 (55.6) |
| Educational status | |||
| Master’s degree or more ‡ | 1383 (30.7) | 639 (32.1) | 744 (29.5) |
| Bachelor’s degree α | 2383 (52.9) | 1086 (54.6) | 1297 (51.5) |
| Secondary/primary | 741 (16.4) | 264 (13.3) | 477 (19.0) |
| Working status | |||
| Employed/self employed | 3001 (66.9) | 1353 (68.0) | 1648 (65.9) |
| Unemployed/retired | 1488 (33.1) | 636 (32.0) | 852 (33.1) |
| Religion | |||
| Christianity | 4042 (89.7) | 1758 (88.4) | 2284 (90.8) |
| Others ᵖ | 462 (10.3) | 230 (11.6) | 232(9.2) |
| Occupation β | |||
| Healthcare sector | 1240 (31.5) | 443 (24.3) | 797 (37.6) |
| Non-healthcare | 1602 (40.6) | 1014 (55.7) | 588 (27.7) |
| Student | 1099 (27.9) | 364 (20.0) | 735 (34.7) |
| †, divorced, separated, widowed and single; ‡ included Masters and PhD; postgraduate, α, diploma and bachelor degree; ᵖ, included Muslims and African traditionalist; β = no response from 610 respondents for this variable (13.4%). SD = standard deviation. Values are numbers (%) except for mean age. |
|||
In order to further reduce bias, this online survey used a Likert scale with provisions for neutral responses so that the answers were not influenced in one way or another. The participants did not receive any incentives; their responses were voluntary and anonymized. Testing for the internal validity of the survey items, the Cronbach’s alpha coefficient score ranged from 0.70 and 0.74, indicating satisfactory consistency.
2.2. Measures
The questionnaire collected data on sociodemographic variables (Table 1), self-assessment of risks about COVID-19, and if they think the public health authorities in their country are doing enough to contain the virus, whether they or any of their close relative was affected by COVID-19, and whether or not they think COVID-19 is real. Other questions relating to knowledge of COVID-19, habits during lockdown, and attitudes towards the infection were included in survey 1, while questions related to knowledge and attitude towards COVID vaccination were included in one of the two surveys. Those questions that were not in both surveys are not included in the current analysis, but the interested reader on these topics is referred to the published articles for a description of items and responses.
2.3. Assessment of risks about COVID-19
Self-assessments of risks about COVID-19 were measured with two items which was common in both surveys. The first item concerned the perception of the risk of being infected by COVID-19 (Q1: “Please rate your risk of being infected with the Coronavirus (COVID-19)”), and the second item was the self-assessment of the risk of dying from the infection (Q2: “Please rate your risk of dying from the Coronavirus (COVID-19) infection”). Each question used a Likert scale with five levels [21]. The scores for each item ranged from 0 (lowest) to 4 (highest). The perceived risk towards COVID-19 score ranged from 0–8 points.
2.4. Ethical consideration
This cross-sectional study was approved by the Human Research Ethics Committee of the Cross River State Ministry of Health, Nigeria (CRSMOH/RP/REC/2020/116) for the first survey, and by the Humanities and Social Sciences Research Ethics Committee (HSSREC 00002504/2021) of the University of KwaZulu-Natal, Durban, South Africa for the second survey. The study adhered to the principles of the Helsinki declaration (as modified in Fortaleza 2013) for research involving human subjects [22]. Prior to the study, an explanation detailing the nature and purpose of the study was provided to all participants using an online preamble. Informed consent was obtained from the participants who were required to answer either a ‘yes’ or ‘no’ to a question on whether or not they were willing to participate in the survey voluntarily. The confidentiality of participants’ responses was assured, and anonymity was maintained. To ensure that only one response per respondent was included in the study per survey, participants were instructed not to take part in the survey at both periods more than once, and, during analysis, we also restricted the data by IP address of the participants.
2.5. Statistical analysis
Continuous variables were summarized using descriptive statistics, including the number of observations used in the calculation (n), mean, and standard deviation (SD), while categorical variables were summarized as counts and percentages of each category for all demographic characteristics for during and post lockdown. To profile the risk of being infected by COVID-19 and the risk of dying from the infection, the Chi-square test was used to determine their prevalence. Each demographic characteristic was compared with a t-test for 2 groups, and one-way analysis of variance (ANOVA) for 3 or more groups. Simple linear regression analysis was used to report the unadjusted coefficient and retained those variables with p value < 0.20 in order to build a multiple linear regression analysis. For multiple linear regression, an elimination procedure was applied to remove non-significant variables (p > 0.05). All analyses were performed using ‘SVY’ commands in STATA/MP V.13.0 (Stata Corp, College Station, TX, USA).
3. Result
3.1. Descriptive statistics
The descriptive statistics of the sociodemographic variables are presented in Table 1,§§ showing the summary of responses from those who participated in the survey during the lockdown and after the lockdown periods. Total responses were a combination of both survey responses. The mean age of the respondents 34.4 ± 11.7 years was similar in both surveys (34.1 ± 11.6 and 34.6 ± 11.8 years, during and post-lockdown respectively). Table 1 shows that most of the respondents were in the 18–28 years age group (38%, n = 1697). There was an almost equal representation of male and female respondents. Most respondents (55.7%, n = 2522) were not married, about half of them (52.9%, n = 2383) completed post-secondary education, and many were employed (66.9%, n = 3001) and worked in a non-healthcare sector (40.5%, n = 1602) at the time of this study. Furthermore, 89.7% of the respondents (n = 4042) were Christians.
Figure 1a and b presents the percentage of responses for the items that make up the dependent variable:) the risk of becoming infected with COVID-19 and the risk of dying from COVID-19 infection, respectively. For each item, the proportion from both surveys who felt either at high or very high risk of contracting the infection was 39.9%, and about a quarter thought they were at risk of dying from the infection. Compared with during lockdown, significantly more respondents felt at high risk [17.12%; 95%CI 16.05–18.24% versus 9.27% 95%CI 8.46–10.15] and very high risk [7.21%, 95%CI 6.49–9.00% versus 5.34%, 95%CI 4.72–6.03%] of becoming infected from COVID-19 post-lockdown. Similarly, 11.76% [95%CI 10.85–12.72%] of respondents felt at high risk of dying from COVID-19 infection after the lockdown compared with 4.92% [95%CI 4.33–5.59%] during the lockdown.
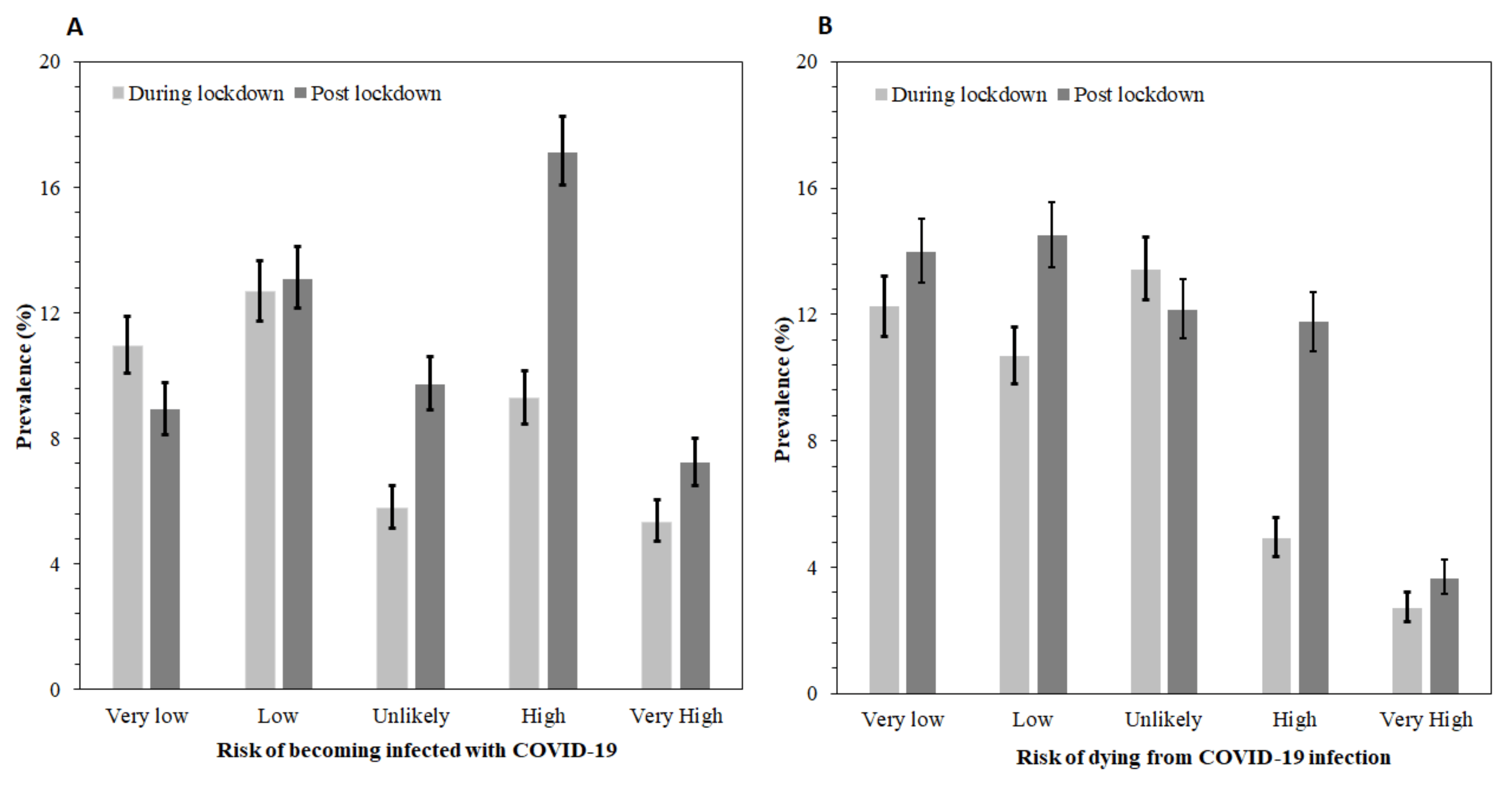
Figure 1. Proportion of responses for perceived risks of COVID-19:
A), the risk of becoming infected with COVID-19;
B) the risk of dying from COVID-19 infection Error bars are 95% confidence intervals. Unlikely means no risk.
3.2. Mean scores and unadjusted factors of risk perception for contracting COVID-19
Figure 2 shows the mean scores for the perceived risk of COVID-19 at 95% CIs (presented as error bars). SSA respondents had significantly higher mean risk perception scores after the COVID-19 lockdown compared with during the lockdown period (p < 0.0005). The perceived risk estimated from the second survey was 0.49 higher than that of the lockdown period. This translates to a Cohen’s D value of 0.21 SD (i.e., the mean of survey 2 and survey 1, and the pooled standard deviation for the entire sample) [23] which was higher than the mean scores of the perceived risk of COVID-19 during the lockdown. From the Emslie data [24], respondents who participated in the post lockdown survey were 58% more likely to perceive a risk of contracting or dying from COVID-19 compared with those that participated in the survey during the lockdown period. This is clinically significant [24].
Table 2 presents the mean risk perception scores as well as the unadjusted odd ratios and their 95% CIs for factors associated with risk perception by the demographic characteristics. Data presented were pooled from both surveys. The mean risk perception scores were significantly different between the study periods. Compared with the lockdown period, the results indicated that perceived risk scores for contracting COVID-19 post-lockdown reduced by 0.49 (95%CI 0.36, 0.63, p < 0.0005) and increased with age. Respondents aged above 28 years had significantly higher risk perceptions scores compared with those aged 18–28 years.
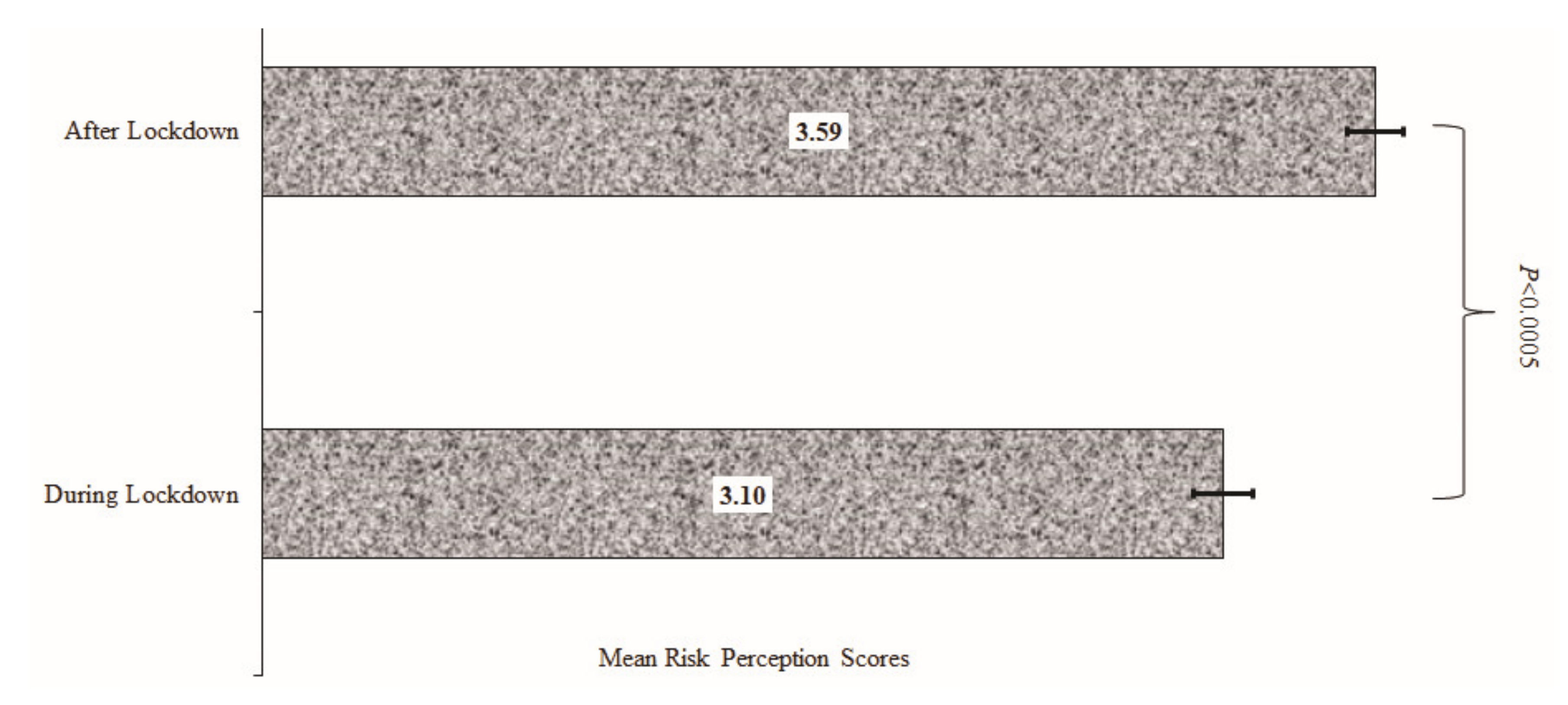
Figure 2. Mean score for the perceived risk of contracting COVID-19 after and during lockdown.
Other factors associated with perceived risk scores for contracting COVID-19 in the unadjusted analysis are region of origin, marital, educational and working status, and respondents’ occupation.
Table 2. Mean scores and unadjusted coefficients (B) for factors associated with perceived risk of contracting COVID-19 during lockdown and post-lockdown.
| Variables | Mean Scores (±SD) | B [95%CI] | p-Value |
|---|---|---|---|
| Survey period | |||
| Period 1 (during lockdown) | 3.10 (2.19) | Ref | |
| Period 2 (post-lockdown) | 3.59 (2.36) | 0.49 [0.36, 0.62] | <0.001 |
| Demography | |||
| Age category in years | |||
| 18–28 years | 3.13 (2.24) | Ref | |
| 29–38 | 3.51 (2.31) | 0.38 [0.22, 0.55] | <0.001 |
| 39–48 | 3.57 (2.35) | 0.44 [0.26, 0.63] | <0.001 |
| 49+ years | 3.58 (2.30) | 0.45 [0.23, 0.66] | <0.001 |
| Sex | |||
| Males | 3.42 (2.32) | Ref | |
| Females | 3.34 (2.27) | −0.08 [−0.22, 0.005] | 0.226 |
| SSA Region of Origin | |||
| West Africa | 3.26 (2.24) | Ref | |
| East Africa | 3.78 (2.41) | 0.51 [0.26, 0.77] | <0.001 |
| Central Africa | 3.22 (2.44) | −0.05 [−0.26, 0.16] | 0.658 |
| Southern Africa | 3.61 (2.30) | 0.35 [0.19, 0.52] | <0.001 |
| Country of residence | |||
| Africa | 3.39 (2.30) | Ref | |
| Diaspora | 3.26(2.23) | −0.13 [−0.40, 0.15] | 0.36 |
| Marital status | |||
| Married | 3.52(2.30) | Ref | |
| Not married | 3.27(2.30) | −0.25 [−0.39, −0.12] | <0.001 |
| Educational status | |||
| Master’s degree or more | 3.50(2.25) | Ref | |
| Bachelor’s degree | 3.37(2.32) | −0.13 [−0.28, 0.02] | 0.089 |
| Secondary/Primary | 3.20 (2.32) | −0.31 [−0.51, −0.10] | 0.004 |
| Working status | |||
| Employed/self employed | 3.54 (2.30) | Ref | |
| Unemployed/retired | 3.10 (2.26) | −0.43 [−0.57, −0.29] | <0.001 |
| Religion | |||
| Christianity | 3.37(2.30) | Ref | 0.676 |
| Others | 3.42(2.29) | 0.05 [−0.17, 0.27] | |
| Occupation | |||
| Healthcare sector | 3.83 (2.34) | Ref | |
| Non-healthcare | 3.20 (2.23) | −0.63 [−0.80, −0.46] | <0.001 |
| Student | 3.09 (2.24) | −0.75 [−0.93, −0.56] | <0.001 |
| SD, standard deviation; CI, confidence interval that do not include 0.00 were significant. SSA, sub-Saharan Africa; Ref, reference (0.00). |
|||
3.3. Factors associated with perceived risk for contracting COVID-19 during lockdown and post-lockdown
Table 3 shows the adjusted coefficients (β) with 95% CIs of the factors influencing perceived risk for contracting COVID-19 during and post-lockdown period in SSA countries. After adjusting for potential confounding factors, the post-lockdown period and age >28 years were significantly associated with increased risk perception. Respondents from East and Southern Africa reported higher risk perception scores compared with those from West Africa. Working in a non-healthcare sector (β −0.56, 95% CI −0.73, −0.38) and being a student (β −0.60, 95% CI −0.82, −0.38) were associated with a reduction in the risk perception scores for contracting COVID-19.
Table 3. Factors associated with perceived risk of contracting COVID-19 in sub-Saharan Africa.
| Variables | β [95%CI] | p-Value |
|---|---|---|
| Year of survey | ||
| Period 1 (during lockdown) | Ref | |
| Period 2 (post-lockdown) | 0.42 [0.27, 0.57] | <0.001 |
| Demography | ||
| Age category in years | ||
| 18–28 years | Ref | |
| 29–38 | 0.25 [0.04, 0.46] | 0.02 |
| 39–48 | 0.31 [0.08, 0.54] | 0.01 |
| 49+ years | 0.31 [0.05, 0.58] | 0.02 |
| SSA Region of Origin | ||
| West Africa | Ref | |
| East Africa | 0.55 [0.28, 0.82] | <0.001 |
| Central Africa | 0.08 [−0.15, 0.31] | 0.49 |
| Southern Africa | 0.37 [0.19, 0.54] | <0.001 |
| Occupation | ||
| Healthcare sector | Ref | |
| Non-healthcare | −0.56 [−0.73, −0.38] | <0.001 |
| Student | −0.60 [−0.82, −0.38] | <0.001 |
| CI, confidence interval that does not include 0.00 were significant. SSA, sub-Saharan Africa; Ref, reference (0.00). β is the adjusted coefficient from the linear regression model. |
||
4. Discussion
To the authors’ ability, this is the first study to compare the level of risk perception of Africans during and after the COVID-19 lockdown period. The study found that more than one in every three persons in this SSA sample and about one in every four respondents felt at high risk of contracting COVID-19 and thought they could die if they contracted COVID-19, respectively, even after the lockdown. Compared with a pre-lockdown period, respondents who participated in the post-lockdown survey reported a significantly higher risk of COVID-19, particularly the older people and respondents that lived in East and Southern Africa. Compared with a pre-lockdown period, respondents who participated in the post-lockdown survey reported a significantly higher risk of COVID-19, particularly the older people, and respondents that lived in East and Southern Africa. The perceived risk of contracting COVID-19 increased significantly between the two surveys showing that respondents overestimated their chances of contracting or dying from COVID-19 by 58%. Although such finding does not reflect a strong deviation from rational behavior, it is common in the literature [25,26], and the likelihood of overestimating small risks fatalities occurs rationally in a Bayesian model when learning is based on partial information [27]. Furthermore, those who worked in health care sectors reported higher risk perception of COVID-19 whereas students who participated in the survey after the lockdown reported lower risk perception compared with other groups.
This increase in risk perception after the lockdown which was found in this study may be attributed to various factors, including the rise in the COVID-19 infections and related deaths in the region after the lockdown [26]. In addition, the controversies surrounding the rolling out of the COVID-19 vaccine globally and the uncertainty of vaccine acceptance in the region [28]. Despite the government efforts at increased sensitization of the populace on the disease, their inability to answer the questions raised about the COVID-19 vaccine [29] could have necessitated the increased risk perception of getting infected after the lockdown.
Past repeat studies have found differences in risk perception of COVID-19 over a time period. A fourth-round survey of respondents in Kenya, East Africa demonstrated that the perceived risk of coronavirus remained about the same, but the proportion that said they are at high risk because they interact with a lot of people every day more than doubled (from 20% to 54%) [30]. In France, two successive representative surveys, one conducted about 2 weeks after lockdown started, and the other about 2 weeks before lockdown ended, found significantly higher risk perception in the second survey than in the first survey. The authors attributed the comparative pessimism in survey 2 to a concomitant increase in the respondents’ perceived chances to contract the disease and a decreased expected prevalence rate [26].
In the present study, we found that older age (≥28 years) was associated with an increased risk of susceptibility to COVID-19; this was consistent with past studies [29,31–33] which showed that older individuals had a higher risk perception of contracting the infection and were more likely to develop more severe complications of COVID-19 or die compared with the younger individuals [32]. The sigh of relief brought about by the post-lockdown era had a serious effect on the younger age groups who, at that time, had a lower risk perception for contracting the infection, as seen in a study by Dillard et al. [30]. The perceived low risk of infection by younger respondents may make them less cooperative and less compliant with the safety measures [34], thus encouraging the spread of the virus while putting a greater part of the population at risk of COVID-19 infections [29,30]. This finding could be attributable to the fact that younger people are the more active age group in any given population.
In his write up about medical students during this COVID-19 era, Flaxman et al. stated that students are not essential workers [35], which implies that they are not yet classified as healthcare workers since they are not paid or tasked with the responsibility of patient care in healthcare facilities [36]. In this study, people working in non-healthcare sectors, including students, felt less susceptible to the infection. This finding can be attributed to exposure of healthcare workers to infected people; the absence of personal protective equipment, particularly in SSA countries [37]; over crowdedness of medical facilities; and inadequate provision of needed health management instruments [37]. There is a need for regular educational intervention and training programs on infection control practices for COVID-19 across all healthcare professions.
The study also found regional differences in the level of perceived risk for contracting COVID-19 during and after the lockdown. Although the risk perception scores were reduced after the lockdown among East Africans, they and Southern Africans felt at greater risk of COVID-19 infection compared with West African respondents. Such regional differences with regard to COVID-19 infection was reported to vary from location to location with significantly varying degrees of impact [38]. In this study, we noted that respondents from two of the participating SSA countries reported higher risk perception scores for contracting the virus, and, for the other two regions—Western and central Africa—the risk perception remained unchanged. Although a cross-sectional study from China did not find a significant regional variation in the risk perception of the SARS-CoV-2 pandemic [39], there are factors that come to play, including the cultural beliefs and inclinations of the people, their religious orientations, the governmental policies in place for the control of the spread of the disease, and the individual tendencies for survival among many others [40].
The study has some limitations which should be interpreted within the context of the study. Using a perceived risk score than ranged from 0–8 points may violate some linear regression assumptions [19,41]. The use of an online survey has the potential to result in selection bias and could have unduly excluded residents in SSA without internet access. The preponderance of educated persons in this study is another limitation that is a characteristic of most survey studies in Africa [19,20,37,42] and elsewhere [43]. These study findings may not be generalizable to the entire SSA of the study findings because not all countries are in SSA answered the questions. Besides these limitations, this is the first study on the knowledge, attitude, and perception of COVID-19 vaccine to include all four SSA regions which also employed comprehensive inferential data analyses.
5. Conclusions
It is clear that, during the lockdown, people had some measure of certainty regarding the SARS-CoV-2, which dissipated after the lockdown as the rates of infection across the globe, particularly in SSA, were seen to be on the surge with a reported increasing number of deaths. Notably, the factors influencing risk perception scores remained the same during and after the lockdown and this included age, region of origin, and occupation. The rollout of the COVID-19 vaccine and the controversies regarding the effectiveness of the vaccines, as well as the media focus on the new variant, may have heightened the perceived risk of infection. There is the need for governments in SSA to intensify the public awareness of the emergence of new variants of the virus and design compatible ways of ensuring that the vaccines are at the reach of everyone and that everyone should be encouraged to recieve his/her shot of the vaccine to stay safe and alive. Furthermore, further studies need to be carried out to ascertain the post lockdown risk perception since, from existent studies, there seems to be non-availability of data on the post lockdown risk perception of contracting SARS-CoV-2 and with the ongoing vaccination in view.
Author contributions: Conceptualization, all authors; Methodology, K.A., U.L.O., T.C.G. and R.L.; Software, K.A., U.L.O.; Validation, T.I., R.O., B.E., O.N., K.P.M., E.K.A., C.A.M., E.A.E. and C.G.T.; Formal Analysis, K.A. and U.L.O.; Investigation, all authors; Resources, all authors; Data Curation, K.A., U.L.O., C.G.T., P.C.G., B.E., K.P.M. and R.L.; Writing—Original Draft Preparation, R.L., P.C.G., U.L.O., E.K.A.; Writing—Review & Editing, T.I., B.E., D.D.C., G.O.O.-O., U.L.O., K.A., K.P.M., E.A.E., C.A.M., J., E.A.E. and C.G.T.; Visualization, K.A., .; Supervision, K.A., U.L.O., T.I., K.P.M.; Project Administration, K.A., U.L.O. and C.G.T. All authors have read and agreed to the published version of the manuscript.
Funding: This research received no external funding
Institutional review board statement: This cross-sectional study was approved by the Human Research Ethics Committee of the Cross River State Ministry of Health, Nigeria (CRSMOH/RP/REC/2020/116) for the first survey and by the Humanities and Social Sciences Research Ethics Committee (HSSREC 00002504/2021) of the University of KwaZulu-Natal, Durban, South Africa for the second survey
Informed consent statement: Informed consent was obtained from all subjects involved in the study.
Data availability statement: The datasets analyzed during this study are available from the authors on reasonable request.
Conflicts of interest: All authors declared no conflict of interest.
Notes
§ https://www.afro.who.int/news/covid-19-deaths-africa-surge-more-40-over-previous-week
# https://www.frontiersin.org/articles/10.3389/fpsyg.2021.619145/full
§§ https://www.frontiersin.org/articles/10.3389/fpsyg.2021.619145/full
References
-
Xia, S.; Liu, M.; Wang, C.; Xu, W.; Lan, Q.; Feng, S.; Qi, F.; Bao, L.; Du, L.; Liu, S. Inhibition of SARS-CoV-2 (previously 2019-nCoV) infection by a highly potent pan-coronavirus fusion inhibitor targeting its spike protein that harbors a high capacity to mediate membrane fusion. Cell Res. 2020, 30, 343–355. [Google Scholar] [CrossRef] [Green Version]
-
Olshaker, M.; Osterholm, M.T. Deadliest Enemy: Our War Against Killer Germs; Hachette: London, UK, 2017. [Google Scholar]
-
COVID-19 Coronavirus Pandemic. Available online: https://www.worldometers.info/ (accessed on 7 October 2021).
-
Chang, S.L.; Harding, N.; Zachreson, C.; Cliff, O.M.; Prokopenko, M. Modelling transmission and control of the COVID-19 pandemic in Australia. Nat. Commun. 2020, 11, 1–13. [Google Scholar] [CrossRef]
-
WHO. Maintaining Essential Health Services: Operational Guidance for the COVID-19 Context: Interim Guidance, 1 June 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
-
Schwartz, J.L. Evaluating and deploying COVID-19 vaccines—The importance of transparency, scientific integrity, and public trust. N. Engl. J. Med. 2020, 383, 1703–1705. [Google Scholar] [CrossRef] [PubMed]
-
OECD.org. Enhancing Public Trust in COVID-19 Vaccination: The Role of Governments. 2021. Available online: https://www.oecd.org/coronavirus/policy-responses/enhancing-public-trust-in-covid-19-vaccination-the-role-of-governments-eae0ec5a/ (accessed on 15 September 2021).
-
Adams, J.; MacKenzie, M.J.; Amegah, A.K.; Ezeh, A.; Gadanya, M.A.; Omigbodun, A.; Sarki, A.M.; Thistle, P.; Ziraba, A.K.; Stranges, S. The Conundrum of Low COVID-19 Mortality Burden in sub-Saharan Africa: Myth or Reality? Glob. Health: Sci. Pract. 2021, 9, 433–443. [Google Scholar]
-
CDC. Older Adults Risks and Vaccine Information Center for Disease Control. 2021. Available online: https://www.cdc.gov/aging/covid19/covid19-older-adults.html (accessed on 15 September 2021).
-
Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef] [PubMed]
-
Gates, B.; Gates, M. Our 2019 Annual Letter—Compact 2025 Resources—IFPRI Knowledge Collections. 2019. Available online: https://ebrary.ifpri.org/digital/collection/p15738coll16/id/1082/ (accessed on 15 September 2021).
-
Adamchak, D.J. Population aging in sub-Saharan Africa: The effects of development on the elderly. Popul. Environ. 1989, 10, 162–176. [Google Scholar] [CrossRef]
-
Jaja, I.F.; Anyanwu, M.U.; Iwu Jaja, C.-J. Social distancing: How religion, culture and burial ceremony undermine the effort to curb COVID-19 in South Africa. Emerg. Microbes Infect. 2020, 9, 1077–1079. [Google Scholar] [CrossRef]
-
Levin, J. The faith community and the SARS-CoV-2 outbreak: Part of the problem or part of the solution? J. Relig. Health 2020, 59, 2215–2228. [Google Scholar] [CrossRef]
-
Buheji, M. Stopping future COVID-19 like pandemics from the Source-A Socio-Economic Perspective. Am. J. Econ 2020, 10, 115–125. [Google Scholar] [CrossRef]
-
Khan, N.; Fahad, S.; Faisal, S.; Naushad, M. Quarantine role in the control of corona virus in the world and its impact on the world economy. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
-
Moti, U.G.; Ter Goon, D. Novel Coronavirus Disease: A delicate balancing act between health and the economy. Pak. J. Med Sci. 2020, 36, S134. [Google Scholar] [CrossRef]
-
Kim, A.W.; Nyengerai, T.; Mendenhall, E. Evaluating the mental health impacts of the COVID-19 pandemic: Perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms in urban South Africa. Psychol. Med. 2020, 1–13. [Google Scholar] [CrossRef] [PubMed]
-
Abu, E.K.; Oloruntoba, R.; Osuagwu, U.L.; Bhattarai, D.; Miner, C.A.; Goson, P.C.; Langsi, R.; Nwaeze, O.; Chikasirimobi, T.G.; Ovenseri-Ogbomo, G.O. Risk perception of COVID-19 among sub-Sahara Africans: A web-based comparative survey of local and diaspora residents. BMC Public Health 2021, 21, 1–13. [Google Scholar] [CrossRef]
-
Ovenseri-Ogbomo, G.O.; Ishaya, T.; Osuagwu, U.L.; Abu, E.K.; Nwaeze, O.; Oloruntoba, R.; Ekpenyong, B.; Mashige, K.P.; Chikasirimobi, T.G.; Langsi, R. Factors associated with the myth about 5G network during COVID-19 pandemic in sub-Saharan Africa. J. Glob. Health Rep. 2020. [Google Scholar] [CrossRef]
-
Maurer, T.J.; Andrews, K.D. Traditional, Likert, and simplified measures of self-efficacy. Educ. Psychol. Meas. 2000, 60, 965–973. [Google Scholar] [CrossRef]
-
Association, W.M. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar]
-
McGough, J.J.; Faraone, S.V. Estimating the size of treatment effects: Moving beyond p values. Psychiatry 2009, 6, 21. [Google Scholar] [PubMed]
-
Emslie, G.J.; Rush, A.J.; Weinberg, W.A.; Kowatch, R.A.; Hughes, C.W.; Carmody, T.; Rintelmann, J. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch. Gen. Psychiatry 1997, 54, 1031–1037. [Google Scholar] [CrossRef]
-
Ferrer, R.A.; Klein, W.M. Risk perceptions and health behavior. Curr. Opin. Psychol. 2015, 5, 85–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
-
Attema, A.E.; L’Haridon, O.; Raude, J.; Seror, V.; The COCONEL Group. Beliefs and Risk Perceptions About COVID-19: Evidence From Two Successive French Representative Surveys During Lockdown. Front. Psychol. 2021, 12, 619145. [Google Scholar] [CrossRef]
-
Viscusi, W.K. Are individuals Bayesian decision makers? Am. Econ. Rev. 1985, 75, 381–385. [Google Scholar]
-
Wouters, O.J.; Shadlen, K.C.; Salcher-Konrad, M.; Pollard, A.J.; Larson, H.J.; Teerawattananon, Y.; Jit, M. Challenges in ensuring global access to COVID-19 vaccines: Production, affordability, allocation, and deployment. Lancet 2021, 397, 1023–1034. [Google Scholar] [CrossRef]
-
Haidere, M.F.; Ratan, Z.A.; Nowroz, S.; Zaman, S.B.; Jung, Y.-J.; Hosseinzadeh, H.; Cho, J.Y. COVID-19 vaccine: Critical questions with complicated answers. Biomol. Ther. 2021, 29, 1–10. [Google Scholar] [CrossRef] [PubMed]
-
COVID-19 Perceptions, Stigma and Impact; Ministry of Health: Nairobi, Kenya, 2020.
-
Clark, A.; Jit, M.; Warren-Gash, C.; Guthrie, B.; Wang, H.H.; Mercer, S.W.; Sanderson, C.; McKee, M.; Troeger, C.; Ong, K.L. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: A modelling study. Lancet Glob. Health 2020, 8, e1003–e1017. [Google Scholar] [CrossRef]
-
Drefahl, S.; Wallace, M.; Mussino, E.; Aradhya, S.; Kolk, M.; Brandén, M.; Malmberg, B.; Andersson, G. A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat. Commun. 2020, 11, 1–7. [Google Scholar] [CrossRef]
-
Dillard, A.J.; Ferrer, R.A.; Welch, J.D. Associations between narrative transportation, risk perception and behaviour intentions following narrative messages about skin cancer. Psychol. Health 2018, 33, 573–593. [Google Scholar] [CrossRef] [PubMed]
-
Franzen, A.; Wöhner, F. Coronavirus risk perception and compliance with social distancing measures in a sample of young adults: Evidence from Switzerland. PLoS ONE 2021, 16, e0247447. [Google Scholar] [CrossRef]
-
Flaxman, A.D.; Henning, D.J.; Duber, H.C. The relative incidence of COVID-19 in healthcare workers versus non-healthcare workers: Evidence from a web-based survey of Facebook users in the United States. Gates Open Res. 2020, 4, 174. [Google Scholar] [CrossRef]
-
Menon, A.; Klein, E.J.; Kollars, K.; Kleinhenz, A.L. Medical students are not essential workers: Examining institutional responsibility during the COVID-19 pandemic. Acad. Med. 2020, 95, 1149–1151. [Google Scholar] [CrossRef]
-
Ekpenyong, B.; Obinwanne, C.J.; Ovenseri-Ogbomo, G.; Ahaiwe, K.; Lewis, O.O.; Echendu, D.C.; Osuagwu, U.L. Assessment of knowledge, practice and guidelines towards the Novel COVID-19 among eye care practitioners in Nigeria—A survey-based study. Int. J. Environ. Res. Public Health 2020, 17, 5141. [Google Scholar] [CrossRef]
-
Allain-Dupré, D.; Chatry, I.; Michalun, V.; Moisio, A. The Territorial Impact of COVID-19: Managing the Crisis Across Levels of Government; OECD: Paris, France, 2020. [Google Scholar]
-
Ning, L.; Niu, J.; Bi, X.; Yang, C.; Liu, Z.; Wu, Q.; Ning, N.; Liang, L.; Liu, A.; Hao, Y. The impacts of knowledge, risk perception, emotion and information on citizens’ protective behaviors during the outbreak of COVID-19: A cross-sectional study in China. BMC Public Health 2020, 20, 1–12. [Google Scholar] [CrossRef] [PubMed]
-
Biddlestone, M.; Green, R.; Douglas, K.M. Cultural orientation, power, belief in conspiracy theories, and intentions to reduce the spread of COVID-19. Br. J. Soc. Psychol. 2020, 59, 663–673. [Google Scholar] [CrossRef] [PubMed]
-
Knief, U.; Forstmeier, W. Violating the normality assumption may be the lesser of two evils. Behav. Res. Methods 2021, 1–15. [Google Scholar] [CrossRef]
-
Osuagwu, U.L.; Miner, C.A.; Bhattarai, D.; Mashige, K.P.; Oloruntoba, R.; Abu, E.K.; Ekpenyong, B.; Chikasirimobi, T.G.; Goson, P.C.; Ovenseri-Ogbomo, G.O. Misinformation About COVID-19 in Sub-Saharan Africa: Evidence from a Cross-Sectional Survey. Health Secur. 2021, 19, 44–56. [Google Scholar] [CrossRef]
-
Abir, T.; Kalimullah, N.A.; Osuagwu, U.L.; Yazdani, D.M.N.-A.; Mamun, A.A.; Husain, T.; Basak, P.; Permarupan, P.Y.; Agho, K.E. Factors Associated with the Perception of Risk and Knowledge of Contracting the SARS-Cov-2 among Adults in Bangladesh: Analysis of Online Surveys. Int. J. Environ. Res. Public Health 2020, 17, 5252. [Google Scholar] [CrossRef] [PubMed]
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
|

